Abstract
Background: Sickle cell disease (SCD) is associated with episodes of vaso-occlusive events (VOE) caused by the effects of hemoglobin S (HbS) polymerization in red blood cells (RBCs) and resultant hemolysis. In the acute setting, treatment for VOE is limited to supportive care such as hydration and aggressive pain management as no specific therapies can alter the course of acute VOE. The apohemoglobin-haptoglobin (apoHb-Hp) complex is a two-protein formulation that is capable of scavenging and neutralizing the toxic effects of cell-free hemoglobin (Hb) and heme released from the hemolysis of polymerized HbS RBCs. The primary objective of this study was to evaluate the microcirculatory effects of apoHb-Hp during hypoxia-induced VOE.
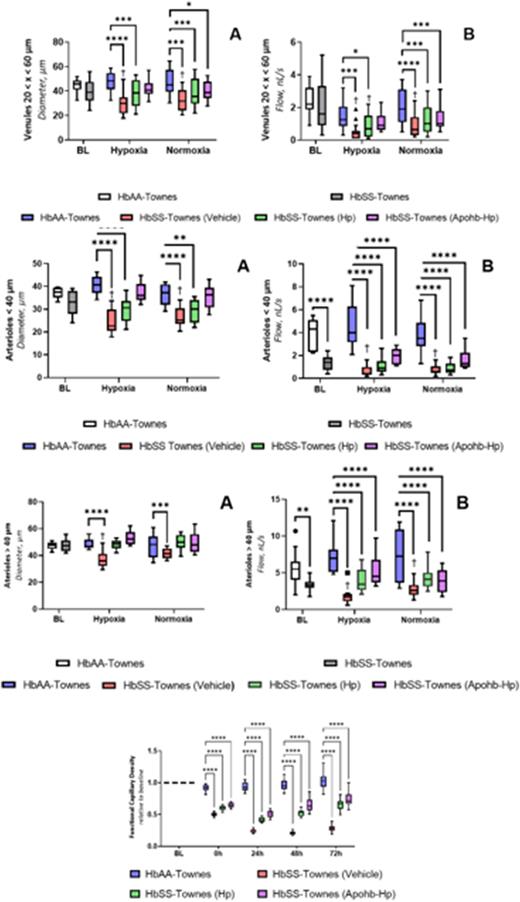
Methods: The effects of apoHb-hp was studied in a mouse model of SCD using sickle cell transgenic mice (HbSS-Towne's mice, and compared to mice expressing normal human Hb (HbAA-Towne's mice). Each group consisted of 11 mice, they were initially kept in normal conditions (21% O2) for an hour followed by a hypoxic state (7% O2) for another hour and finally brought back to normal conditions (21% O2) for an hour before being sacrificed. ApoHb-hp (60 mg/mL) and Hp (85 mg/mL) were injected intravenously to yield equimolar total heme and Hb binding capacity between treatments prior to hypoxia exposure. During baseline, hypoxia and normoxia systemic parameters (mean arteriole pressure and heart rate), blood gases (pO2,A, pO2,v, sO2,A, sO2,v), hematological properties (total Hb concentration, hematocrit, and concentration of lactate) and microcirculatory hemodynamics (velocity, diameter, flow and functional capillary density) were measured. After the mice were sacrificed a count of present macrophages, neutrophils and lymphocytes were quantified in the pulmonary tissue.
Results: There was no notable changes in blood gas concentrations with any of the treatments. ApoHb-Hp treatment improved microcirculatory hemodynamics of HbSS mice by preventing hypoxia-induced vasoconstriction and reduction of blood flow in arterioles <40µm (P=0.818, P<0.0001), arterioles >40 µm (P>0.9999, P<0.0001) and venules 20<x<60 µm (P=0.150, P=0.330) compared to HbAA mice. Furthermore, the functional capillary density saw favorable recovery to baseline when HbSS mice were treated with apoHb-Hp seeing a 36% drop initially, 50% drop after 24 hours, 35% drop after 48 hours, and 27% drop after 72 hours. For comparison, HbSS mice that didn't receive treatment saw a 50% drop initially, 77% drop after 24 hours, 80% drop after 48 hours, and 72% drop after 72 hours when compared to baseline.
Conclusion: These results suggest a role for ApoHb-Hp complex in alleviating microvascular changes occurring during hypoxia mediated acute vaso-occlusion in SCD and merits further study for development as a potential therapeutic.
Disclosures
Munoz:Global Blood Therapeutics: Research Funding. Muller:Global Blood Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal